COVID-19 and the Immune System of Children and Adults
Information about rare coronavirus-related syndrome in kids, courtesy of New York City Health
COVID-19 and the Immune System of Adults and Children
My PhD is in the field of immunology. Thirty years ago I took an immunology class at MIT and I was hooked. (If you’re ever at a party with me and you’re sufficiently intoxicated, ask me about the generation of antibody diversity.)
Extraordinary doesn’t begin to describe the complexity and genius of the human immune system. But as with any complex system, regulation is vital. When it goes wrong, it can go very wrong. Your immune system is like a vast military-industrial complex with the power to dispatch armies, manufacture missiles, plant minefields, and drop bombs. As in the real world, there’s risk of collateral damage, of friendly fire, even of mutually assured destruction.
Evidence is growing that immune system dysfunction is an important contributor to the clinical disease we call COVID-19. The virus SARS-CoV-2 damages the body but the immune system’s assault on the virus causes damage too—maybe worse.
How does that happen? You’ve heard the term inflammation. Inflammation is a major weapon of the immune system. It’s also a threat to health in a variety of ways. Unlike antibodies, inflammation is nonspecific. It includes chemicals called cytokines (and others) that spill out of cells and flood your body. Dying cells cry for help and trigger inflammation, and white blood cells run into battle. Like an aerial bombing raid, inflammation is great when it hits the desired target. It’s not so great when the enemy has retreated but you nuke the village anyway.
The SARS-CoV-2 virus infects cells of the deep lungs, or “lower respiratory tract.” As I explained in this post, viruses invade cells and then use the cell as a factory to manufacture more viruses. One way or another, this often ends in the death of the cell. So SARS-CoV-2 can directly damage the lungs. But in COVID-19, a lot of the lung damage is from inflammation–a self-inflicted wound. According to this excellent article in Nature Reviews Immunology:
“aggressive inflammatory responses {are} strongly implicated in the resulting damage to the airways. Therefore, disease severity in patients is due to not only the viral infection but also the host response.“
That’s not the only immune-related problem in COVID-19. Again, from the same review article:
“respiratory failure … is the cause of death in 70% of fatal COVID-19 cases. In addition, the vast release of cytokines by the immune system in response to the viral infection and/or secondary infections can result in a cytokine storm and symptoms of sepsis that are the cause of death in 28% of fatal COVID-19 cases. In these cases, uncontrolled inflammation inflicts multi-organ damage leading to organ failure, especially of the cardiac, hepatic and renal systems.”
In other words, the patient’s inflammatory response extends beyond the original site of infection in the lungs, and attacks other organs too. The immune-mediated damage can be severe enough to kill. (For a little more tech, here’s a nice report about the innate vs adaptive immune response in COVID-19.)
Better therapeutic target
This is actually good news. Powerful antiviral drugs are hard to come by. But we already have a wide range of pharmaceuticals that affect the immune system. If an overreaction by the immune system is a big part of what COVID-19 patients die from, then better treatments for COVID could be within reach.
“Several immunosuppressive therapies aimed at limiting immunomediated damage in COVID-19 are at various phases of development and are listed in Table 1.” (Nature Reviews)
Furthermore, a person’s genes probably account for some, or most, of their risk for an immune overreaction. Scientists are looking at COVID patients’ genomes to try to find DNA markers that are associated with this increased risk. If we can identify these patients before they end up on a ventilator, doctors can adjust their treatment to be more aggressive at suppressing a cytokine storm before it happens.
Aside: The ability to moderate the inflammatory response may be the key reason why bats are tolerant of many viruses that are deadly in other mammalian species. (Read my post.)
What about kids?
As I’ve reported several times, for all intents and purposes children are not dying of COVID-19. It’s an incredible blessing in this pandemic. SARS-CoV-2 infections in minors appear to be largely mild or asymptomatic. Why? We don’t know for sure, but probably it has something to do with the immune component to the disease. The immune system in kids behaves differently than in adults or the elderly. Those differences may mean children infected by SARS-CoV-2 don’t get the same inflammation in their lungs, so they don’t end up with respiratory distress.
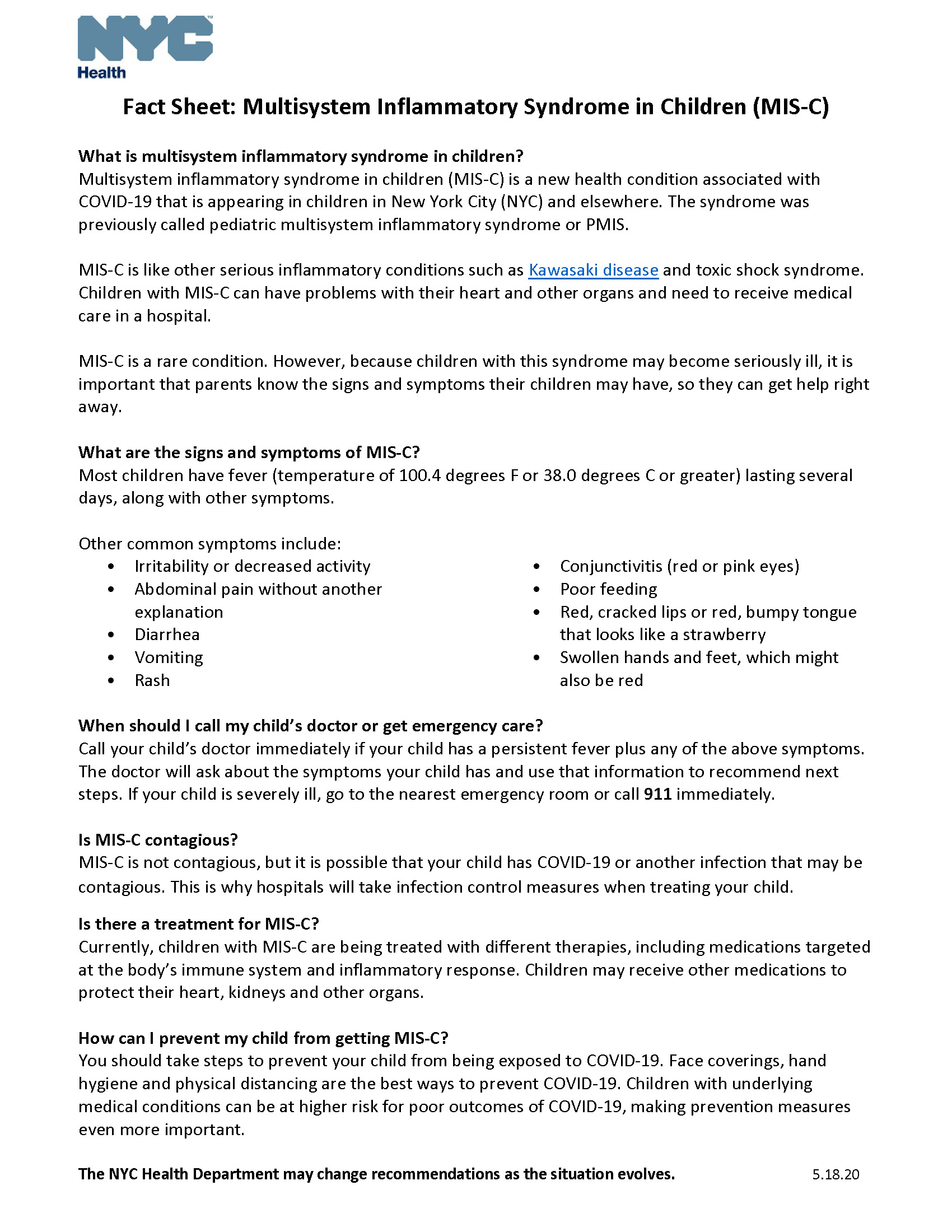
However we do have some bad news on this front. If enough kids catch the coronavirus, a tiny fraction of them develop a serious immune complication. Doctors in New York picked up on it a few weeks ago (yay, docs!) The CDC is calling it “multisystem inflammatory syndrome in children associated with COVID-19.” The initial coronavirus infection can be mild or with no symptoms at all. Nevertheless weeks later, the child’s immune response has continued to produce inflammation that can cause fever and a variety of symptoms around the body (see notes in image at top).
In severe cases, inflammation of organs like the heart may require hospitalization. Kids are resilient and doctors have experience treating similar conditions in children, so full recovery is the norm. SARS-CoV-2 is not the first virus known to trigger a delayed inflammatory syndrome in children. The table below lists other viruses that have been shown to do something similar, and an inflammation of the heart called Kawasaki disease may be triggered by a virus that hasn’t been identified yet. In fact doctors thought the first cases were Kawasaki disease, but most of these kids tested positive either for SARS-CoV-2 virus or for antibodies indicating recent infection.
I want to emphasize that recognizing this inflammatory syndrome is an important achievement in our understanding of the pandemic, but as a professor at Stanford Children’s Health says, “We want to reassure families that this complication is very rare.”
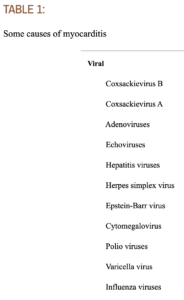 Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805590/
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805590/
To view CDC Health Alert about MIS-C, click here
For an excellent Atlantic article about MIS-C, click here.
Amy Rogers, MD, PhD, is a Harvard-educated scientist, novelist, journalist, and educator. Learn more about Amy’s science thriller novels, or download a free ebook on the scientific backstory of SARS-CoV-2 and emerging infections, at AmyRogers.com.
Sign up for my email list
Share this:
0 Comments