Pandemic Progress Report: California, June 24

Pandemic Progress Report: Sacramento California, June 24
Hold tight. The coronavirus is on the move.
Back during shelter-in-place days, hubby and I would talk about how the pandemic felt like something that was happening to other people in other places. We mused about how easily people could deny that the new coronavirus existed, or to downplay the risk to themselves or their town, because so few Americans actually knew anyone with COVID-19. We didn’t have a personal connection to anyone infected by SARS-CoV-2.
Times are changing—fast.
In just over a week we’ve gone from not knowing anyone with coronavirus to having friends in two unconnected households from our Christmas card list testing positive, plus an important colleague, plus a roommate of a friend of one of our children. Of those four people, all had symptoms to some degree. So far none have been sick enough to need hospitalization.
The official numbers for Sacramento reflect this personal experience. The county is experiencing record numbers of new infections. Four days ago, we set a single-day record of 93 diagnosed cases. Yesterday, a new record: 131 lab-confirmed infections.
According to the Sacramento Bee, “Sacramento County has now reported 2,374 total cases of COVID-19, and over 390 of them have been disclosed by the county since Saturday. That’s more than 16 percent of the all-time infection total, which dates back to February. More than 5 percent came Tuesday alone.”
How much is too much?
Clearly the virus is spreading. We expected that. When we came out of our homes and started engaging in commerce and activities again, of course there would be more exposures, and more infections. So at what point do we have a problem that demands more action?
There are a couple of ways to look at this. I’m going to talk specifically about Sacramento County. An important point is that the pandemic varies wildly from place to place. The specifics will be different where you are, but the issues are the same.
Hospitals: The goal of lockdown was to flatten the curve. Remember, that meant we were keeping the number of cases low enough that the health care system would not be overwhelmed. In the US, we largely achieved this everywhere except the NY metropolitan area. This continues to be the one thing everyone agrees on: COVID-19 hospitalizations must not exceed our system’s capacity to give the best care possible to every patient.
As of today, Sacramento County has 19 COVID patients in intensive care. This is a small number relative to capacity; at the moment local hospitals have over 160 empty ICU beds and 500 available ventilators. So Sacramento has plenty of room. The danger, however, is that hospitalizations lag infections by several weeks. By the time the ICUs are full, it’s too late to make the necessary changes in infection rates.
Based on what we see today, can we predict where we’ll be with the local epidemic in one, two, or three weeks’ time? This is what epidemiologic modeling is for. Unfortunately modeling this pandemic hasn’t been very accurate because mathematical models are only as good as the assumptions built into them—and the assumptions about this virus are often guesses. What we can see is that doubling times are getting shorter here and elsewhere. Because an epidemic grows exponentially, the safe option is to take action to curtail it early. We should emphasize and enforce the easiest, cheapest non-pharmaceutical interventions (NPIs) first, things like handwashing, physical distancing, and wearing masks. This is what California Governor Newsom did this week when he made face coverings mandatory statewide basically for anyone who is indoors, or outdoors and unable to keep 6 feet away from people they don’t live with. Masks are easy, cheap, and they do some good.
Should we close parts of the newly reopened economy? Not yet, at least not here. But we must pay attention to…
Trends: Where is the virus spreading? In Sacramento, data obtained from contact tracing blames most new clusters on a failure to follow the current guidelines and NPIs. Too many people seem to view lockdown/opening as all or nothing. Businesses reopened, so people started having gatherings inside their homes. Cases came from in-home birthday and graduation parties, not nail salons. A mistake!
Trends: Who is getting infected? In my Coronavirus Endgame series of posts, I hammered on the idea that the pandemic ends with herd immunity. The only question is, how do we get there. Will herd immunity happen by natural infection, or a combination of natural infection plus a vaccine? Will it happen quickly or gradually?
Vaccination is best, of course, but the timeline for success is unknown.
Natural infection is good for some groups of people but terrible for others. It is never 100% risk free.
Back in April I advocated re-opening for people at low risk of death from COVID-19 so that they could start to build the firewall of herd immunity that will ultimately protect the most vulnerable. Now, the identity of those people is as clear as ever: they’re young or middle-aged, and healthy.
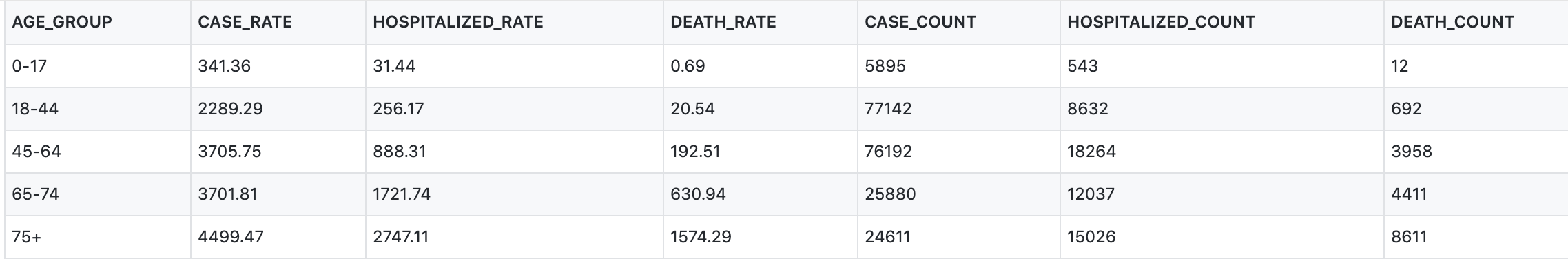
Data from New York City health department (tables; rates are per 100,000 New Yorkers) and Sacramento County Public Health (bar graphs), as of June 24, 2020
Sacramento has a preponderance of positive coronavirus tests among the young, but an overwhelming majority of COVID-19 deaths among people over age 65.
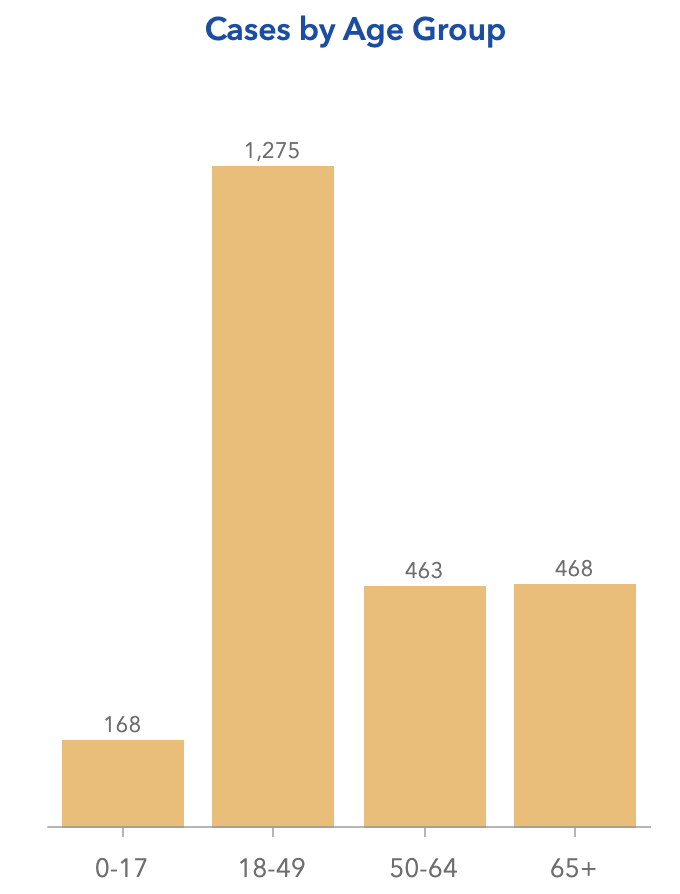
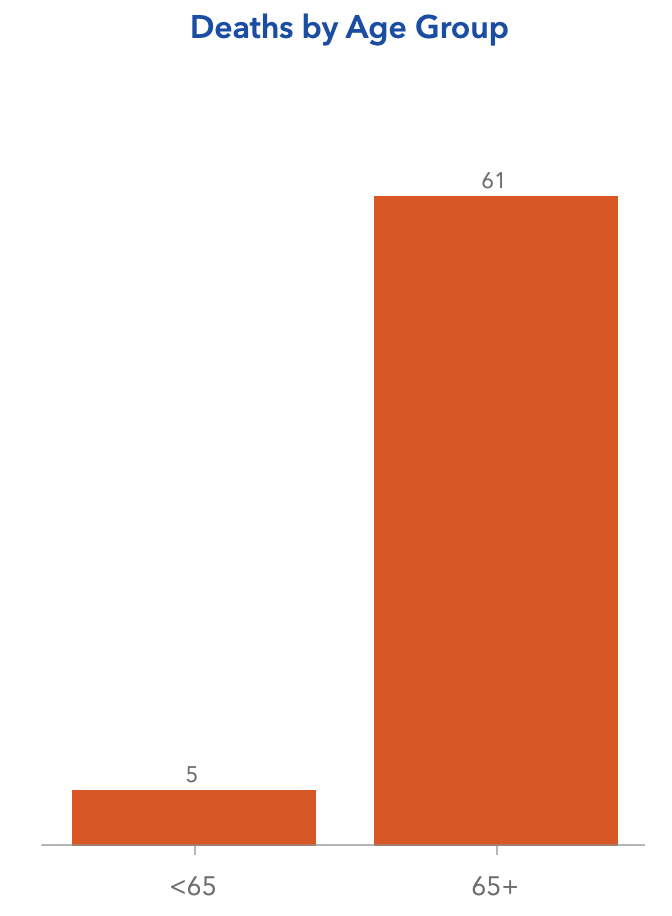
New York City data are more detailed and even more impressive. An 80-year-old New Yorker was something like 2,300 times more likely to die of a coronavirus infection than an infected 17-year-old. Factor in pre-existing health problems and the chance of a healthy person under the age of 45 dying from SARS-CoV-2 infection is very, very small. Even in the 45-64 age group, mortality for previously healthy people who test positive for coronavirus is in the range of only 1 to 3 per thousand infections.
Hospitalization rates are also skewed by age, though not as severely. A hundred new infections among people age 65+ translates into about 8 times as many hospitalizations as a hundred new infections among under-45s.
Here’s the takeaway:
Rising numbers of positive coronavirus tests in many parts of the US bear close watching, but they’re not the whole story. Is the virus primarily circulating among teens, 20s and 30-somethings? Or is it spreading among the elderly? Appropriate action is different for these scenarios.
IF seniors and other people at risk can be protected from exposure, we can handle a lot of corona-positive youngsters.
Johns Hopkins Center for Health Security COVID-19 Daily Update (subscribe here), one of my trusted sources, says this may be happening.
“US COVID-19 AGE SHIFT The US COVID-19 incidence continues to increase, since early June, coinciding with states’ efforts to relax social distancing and resume normal activities, but US COVID-19 deaths have steadily decreased since mid-April. One potential explanation for these differing trends is a shift in age distribution of COVID-19 patients toward younger age groups. Several states that are currently reporting surges in COVID-19 incidence—including Arizona, California, Florida, Texas, and Washington—have exhibited an increasing proportion of cases among younger adults (eg, in their 20s and 30s).”
The newsletter goes on to point out the risk, however:
“While many of the newly identified COVID-19 cases may be among younger individuals who are at lower risk for severe disease and death, any increase in cases in the community increases transmission risk, including to higher-risk individuals. Some health experts view the shift toward younger cases as an “ominous” signal that could forecast future increases in severe disease and death as transmission spreads beyond younger demographic groups.”
As is usual in this pandemic, we are left with some data, lots of uncertainty, and difficult trade-offs.
Do your part to protect the vulnerable and to keep the economy open. Observe NPIs as a service to your community even if you feel personally safe.
———————————–
PS: Note that I did not list deaths as a metric to use for any decision to lock down the economy. This is mainly because deaths lag way too far behind. Infections are detected days/weeks after exposures; hospitalizations increase days/weeks after infections; and deaths follow hospitalizations by yet more days/weeks. If you wait until bodies are piling up to take action, you’re in big trouble because no matter what you do, you won’t see a benefit for a long time.
PPS: In my discussion here, I focused on mortality rates and hospitalizations. I acknowledge that there is another adverse outcome: COVID survivors who experience long-term disability. I have not seen data on this subset so I do not know how common it is in either the young or the old. If you know a place on the internet where such data are available, please let me know.
Amy Rogers, MD, PhD, is a Harvard-educated scientist, novelist, journalist, and educator. Learn more about Amy’s science thriller novels, or download a free ebook on the scientific backstory of SARS-CoV-2 and emerging infections, at AmyRogers.com.
Sign up for my email list
Share this:

0 Comments